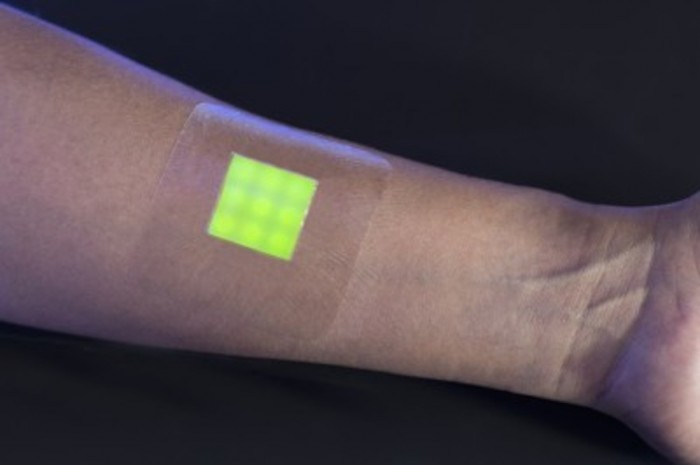
A team of researchers at the University of Bath in the UK have designed a prototype for a burn dressing that changes colour when the patient’s wound is infected. If successful, the smart dressing could dramatically decrease the use of antibiotics and increase the chance for early treatment of infection.
The innovation comes just as the World Health Organisation (WHO) dubbed antibiotic resistance a global health crisis. Antibiotic resistance happens when bacteria become immune to existing drugs, allowing otherwise minor injuries and common infections to become deadly.
While antibiotic resistance happens naturally over time, the overuse of antibiotics in modern healthcare has sped up the process significantly. But detecting the infection early, or detecting that there is no infection at all, will decrease the use of antibiotics when treating burn victims.
“This new dressing technology will not only help clinicians provide the best possible treatment for patients with burns, but could also tell us a lot about how wound infections begin and how they affect the normal healing process. This could in turn lead to even further advances in treating these infections,” says Dr Brian Jones, Reader in Molecular and Medical Microbiology from the University of Brighton.
According to Dr Toby Jenkins, one of the leaders in Biophysical Chemistry at Bath University, the medical dressing works by releasing fluorescent dye from nanocapsules triggered by the toxins secreted by disease-causing bacteria within the wound.
“The nanocapsules mimic skin cells in that they only break open when toxic bacteria are present; they aren’t affected by the harmless bacteria that normally live on healthy skin,” he adds. “Using this dressing will allow clinicians to quickly identify infections without removing it, meaning that patients can be diagnosed and treated faster. It could really help to save lives.”
The team were awarded £1 million by the Medical Research Council, through the Biomedical Catalyst funding stream, and will now begin the next phase of development – testing the responsiveness of the prototype dressing using samples taken from the wounds of burn victims.