Malaria is a global epidemic affecting 200 million people every year. It is considered to be one of the deadliest in the world – the World Health Organisation (WHO) reported that about 438 000 people died from malaria (2015) mainly in sub-Saharan Africa. The deadly disease is caused by a parasite that is spread by certain mosquitos from person to person and can go undetected in its early stages as it often resembles flu-like symptoms. It is therefore vital that the disease is detected early, but sadly it often happens to late and mostly as a result of high medical costs.
Twenty-six-year-old PhD student at MIT, John Lewandowski echoes that early diagnosis is critical, "Early detection is very important, typically in the first five to seven days before symptoms arise, so that treatment can begin." The forward-thinker has designed a mechanical malaria-detecting device called RAM (Rapid Assessment of Malaria) that can detect malaria from a single drop of blood in only five seconds.
Malaria can be diagnosed in two ways: by testing a drop of blood under a microscope to verify the presence of the parasite, or by way of a diagnostics test on a blood test sample – this acts in a similar manner as a home pregnancy test; returning a positive or negative result. The challenge with these primary methods lie in the fact that in Asia and Africa’s rural communities there aren’t medical infrastructure in place to perform microscopic and diagnostic tests. This means that early detection isn’t possible for these communities.
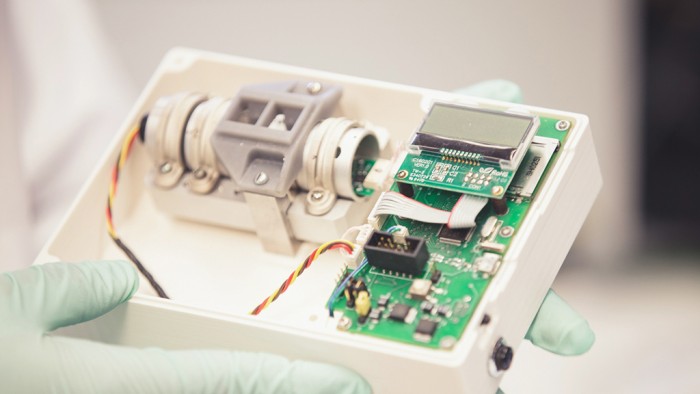
The RAM device
Made from affordable materials, the RAM device costs in the region of R1400 to R1700. The 10 cm by 10 cm plastic box features a small circuit board, magnets and a laser. An LCD screen, SD card slot and a plastic disposable cuvette (a straight-sided clear container for holding liquid samples) frames the outside. "It's pretty bare bones," said Lewandowski, who's the founder and CEO of Boston-based Disease Diagnostic Group, which is developing the device. When present in human blood, malaria parasites form iron crystals called hemozoin – a by-product that the parasites leave in their wake as they destroy red blood cells – that are magnetic. "As an engineer, I thought about creating a way to detect these magnetic crystals quickly," said Lewandowski.
How RAM works
The device uses a magneto-optical detection method. A person takes a finger prick of blood and inserts it into RAM by way of the cuvette. If there is a presence of the Malaria parasite in the blood, the magnets draw the iron crystals horizontally, diagonally or vertically. This creates definitive patterns of the pigment in the blood sample. Next, the laser is shined through the blood sample measuring the percentage of light that passes through the sample. This helps to identify the pattern and ultimately accurately diagnose the disease and commence with the treatment appropriate to the severity of the disease. If the malaria parasite isn’t present in the blood, no crystals will form. Although the technology is purposefully simple, detailed diagnostics and treatment determination must still be performed by a clinic or hospital.
"The technology is novel," said David Sullivan, a professor at Johns Hopkins University and an expert on hemozoin. Sullivan noted that it offers a slight advantage over other rapid diagnostic tests due to its speed as sometimes malaria patients can die within 24 hours. Lewandowski explains that his malaria-detecting device isn’t attempting to reinvent the wheel. "Our technology is just speeding up that same process and bringing down the cost," he said. Lewandowski’s company, Disease Diagnostic Group ran clinical trials in India in 2013 and in the 250-patient study a 93 to 97 percentage accuracy was achieved. The company is exploring ways in which RAM can be adapted to test for other mosquito-borne diseases such as dengue fever and the Zika virus.
It is Lewandowski’s pursuit to eventually place RAM in the communities in high-risk malaria territories. "For us, social impact is our mission," he said. "We want them to be used in the right way by the right people who need them the most."